Careful assessment is an important part of evidence-based practice. Initial assessments of depressive symptoms can help determine possible treatment options, and periodic assessment throughout care can guide treatment and gauge progress.
Many of the instruments described below were used in the studies that served as the evidence base of the systematic reviews that undergird the guideline recommendations. These instruments include both interview and self-report measures and may be used to screen, diagnose and/or track treatment outcomes. Each instrument has been demonstrated to be valid and reliable, and most are available at no cost.
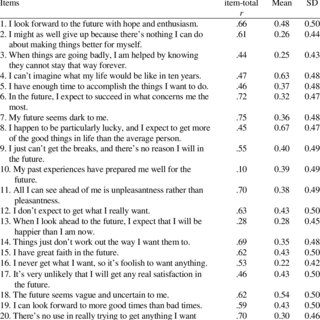
Beck Hopelessness Scale. December 17, 2020. Beck Anxiety Inventory (Urdu) December 17, 2020. Conduct Disorder Rating Scale- for Parents. RS 14 -Resilience Scale 14 items questionnaire. Hi,Can you mention which scale you got? Beck's Depression Inventory. This depression inventory can be self-scored. The scoring scale is at the end of the questionnaire. 0 I do not feel sad. 1 I feel sad 2 I am sad all the time and I can't snap out of it. 3 I am so sad and unhappy that I can't stand it. 0 I am not particularly discouraged about the future. This powerful predictor of eventual suicide assists you to measure three major aspects of hopelessness: feelings about the future, loss of motivation, and expectations. Responding to the 20 true or false items on the Beck Hopelessness Scale (BHS), patients can either endorse a pessimistic statement or deny an optimistic statement.
Clinicians are encouraged to review the evidence-based literature about these assessments, especially regarding their intended use and appropriate populations, in order to determine which tools are best suited for their patients and practices.
Across the Lifespan
The Beck Depression Inventory (BDI) is widely used to screen for depression and to measure behavioral manifestations and severity of depression. The BDI can be used for ages 13 to 80. The inventory contains 21 self-report items which individuals complete using multiple choice response formats. The BDI takes approximately 10 minutes to complete. Validity and reliability of the BDI has been tested across populations, worldwide.
Beck, A.T., Ward, C.H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561-571. http://dx.doi.org/10.1001/archpsyc.1961.01710120031004
Beck, A.T., Steer, R.A., & Brown, G.K. (1996). Manual for the Beck Depression Inventory-II. San Antonio: Psychological Corporation.
Osman, A., Kopper, B.A., Barrios, F., Gutierrez, P.M., & Bagge, C.L. (2004). Reliability and validity of the Beck Depression Inventory—II with adolescent psychiatric inpatients. Psychological Assessment, 16(2), 120-132. http://dx.doi.org/10.1037/1040-3590.16.2.120
More Information
How to Access
- Pricing varies and can be purchased through Pearson Assessments.
Center for Epidemiologic Studies Depression Scale (CES-D)
The Center for Epidemiologic Studies Depression Scale (CES-D) was designed for use in the general population and is now used as a screener for depression in primary care settings. It includes 20 self-report items, scored on a 4-point scale, which measure major dimensions of depression experienced in the past week. The CES-D can be used for children as young as 6 and through older adulthood. It has been tested across gender and cultural populations and maintains consistent validity and reliability. The scale takes about 20 minutes to administer, including scoring.
Radloff, L.S. (1977). The CES-D Scale: A self-report report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385-401. http://dx.doi.org/10.1177/014662167700100306
Saracino, R.M., Cham, H., Rosenfeld, B., & Nelson, C.J. (2018). Confirmatory factor analysis of the Center for Epidemiologic Studies Depression Scale in oncology with examination of invariance between younger and older patients. European Journal of Psychological Assessment. Advance online publication. http://dx.doi.org/10.1027/1015-5759/a000510
More Information
How to Access
- The CES-D (PDF, 28KB) is in the public domain and no permission is required for use.
The EQ-5D is a standardized, non-disease specific instrument for describing and evaluating health-related quality of life. The instrument measures quality of life in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. It was introduced as a health-related quality of life measure by a group of European researchers, the EuroQol Group. Respondents can complete the questionnaire in under five minutes. There is a version for adults (age 16 and older) and the EQ-5D-Y for children/adolescents (8 to 15 years). The EQ-5D is available in a wide range of languages and is used worldwide.
The EuroQol Group (1990) EuroQol — A new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199-208. https://doi.org/10.1016/0168-8510(90)90421-9
Brooks, R., & EuroQol Group (1996).EuroQol: The current state of play. Health Policy, 37(1), 53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6
Devlin, N.J., & Brooks, R. (2017). EQ-5D and the EuroQol group: Past, present and future. Applied Health Economics and Health Policy, 15(2), 127-137. https://doi.org/ 10.1007/s40258-017-0310-5
More Information
How to Access
- Samples and demos of the EQ-5d are available at EuroQol.
The Hamilton Rating Scale for Depression, abbreviated HDRS, HRSD or HAM-D, measures depression in individuals before, during and after treatment. The scale is administered by a health care professionals and contains 21 items, but is scored based on the first 17 items, which are measured either on 5-point or 3-point scales. It takes 15 to 20 minutes to complete and score.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery & Psychiatry, 23, 56-61. http://dx.doi.org/10.1136/jnnp.23.1.56
Trajković, G., Starčević, V., Latas, M., Leštarević, M., Ille, T., Bukumirić, Z., & Marinković, J. (2011). Reliability of the Hamilton Rating Scale for Depression: A meta-analysis over a period of 49 years. Psychiatry Research, 189(1), 1-9. http://dx.doi.org/10.1016/j.psychres.2010.12.007
More Information
How to Access

- The HAM-D (PDF, 22KB) is in the public domain and no permission is required for use.
The 10-item Montgomery-Åsberg Depression Rating Scale (MADRS) measures severity of depression in individuals 18 years and older. Each item is rated on a 7-point scale. The scale is an adaptation of the Hamilton Depression Rating Scale and has a greater sensitivity to change over time. The scale can be completed in 20 to 30 minutes.
Montgomery, S.A., & Åsberg, M. (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134, 382-389. http://dx.doi.org/10.1192/bjp.134.4.382
Davidson, J., Turnbull, C.D., Strickland, R., Miller, R., & Graves, K. (1986). The Montgomery‐Åsberg Depression Scale: Reliability and validity. Acta Psychiatrica Scandinavica, 73(5), 544-548. https://doi.org/10.1111/j.1600-0447.1986.tb02723.x
More Information
How to Access
- The MADRS (PDF, 185KB) is in the public domain and no permission is required for use.
The scale, including all developments and translations, is copyright: © Stuart Montgomery 1978, Measures of Depression, Fulcrum Press, London.
Social Problem-Solving Inventory-Revised (SPSI-RTM)
The Social Problem-Solving Inventory-Revised (SPSI-RTM) is a self-report measure of social problem-solving strengths and weaknesses in individuals 13 years old and older. The revised version has both a long form (52 questions) and short form (25 questions). It takes 10 to 20 minutes to complete.
D'Zurilla, T.J., & Nezu, A.M. (1990). Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 2(2), 156-163. http://dx.doi.org/10.1037/1040-3590.2.2.156
D'Zurilla, T.J., Nezu, A.M., & Maydeu-Olivares, A. (2002). Social problem-solving inventory — revised (SPSI-R). North Tonawanda, New York: Multi-Health Systems.
More Information
How to Access
- Pricing varies and can be purchased through MHS Assessments.
Children and Adolescents
Behavior Assessment System for Children (BASC)
Designed to assess emotional disorders, personality constructs and behavioral problems in individuals from 2 to 21 years old, the BASC assesses behavior from three perspectives: teacher, parent and self (starting at age 8). The system includes five rating forms and three scales. Depending on the scale, it takes 20 to 30 minutes to administer.
Merenda, P.F. (1996). BASC: Behavior Assessment System for Children. Measurement and Evaluation in Counseling and Development, 28(4), 229-232.
Reynolds, C.R., & Kamphaus, R.W. (2015). Behavior assessment system for children (3rd ed.). Bloomington, Minnesota: Pearson Assessments.
Merenda, P.F. (1996). BASC: Behavior Assessment System for Children. Measurement and Evaluation in Counseling and Development, 28(4), 229-232.
Reynolds, C.R., & Kamphaus, R.W. (2015). Behavior assessment system for children (3rd ed.). Bloomington, Minnesota: Pearson Assessments.
More Information
BASC3 Copyright © 2015 NCS Pearson, Inc. Reproduced with permission. All rights reserved.
3.2. BASC is a trademark, in the U.S. and/or other countries, of Pearson Education, Inc. or its affiliates(s).
How to Access
- Pricing varies and can be purchased through Pearson Assessments.
The Child Behavior Profiles were designed for children and adolescents ages 6 to 18. The Child Behavior Checklist (CBCL) is a standardized questionnaire administered to parents to obtain reports of their children’s social competence and behavioral problems. It takes parents five to 10 minutes to complete the questionnaire. Additional versions are available, including the Teacher’s Report Form and Youth Self-Report (from age 11). The CBCL has been translated into various languages.
Achenbach, T.M. (1978). The child behavior profile: An empirically based system for assessing children’s behavioral problems and competencies. International Journal of Mental Health, 7(3-4), 24-42. https://doi.org/10.1080/00207411.1978.11448806
Kariuki, S.M., Abubakar, A., Murray, E., Stein, A., & Newton, C.R.J.C. (2016). Evaluation of psychometric properties and factorial structure of the pre-school child behaviour checklist at the Kenyan Coast. Child and Adolescent Psychiatry and Mental Health, 10, Article ID 1. http://dx.doi.org/10.1186/s13034-015-0089-9
More Information
How to Access
- Contact ASEBA for pricing.
The Children’s Depression Inventory is a modification of the Beck Depression Inventory for adults. The CDI is now on its second edition. It assesses depression severity in children and adolescents 7 to 17 years old. Two scales measure emotional problems and functional problems. Three separate rater forms are available: one for parents (17 items), one for teachers (12 items) and a self-report (28 items). Administration time is between five and 15 minutes.
Kovacs, M. (1981). Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica: International Journal of Child & Adolescent Psychiatry, 46(5-6), 305-315. http://dx.doi.org/10.1037/t00788-000
Sun, S., & Wang, S. (2015). The children’s depression inventory in worldwide child development research: A reliability generalization study. Journal of Child and Family Studies, 24(8), 2352-2363. https://doi.org/10.1007/s10826-014-0038-x
More Information

Used by permission from Multi-Health Systems, Inc.
How to Access
- Pricing varies and can be purchased through Pearson Assessments.
The Children’s Depression Rating Scale (CDRS) was originally designed to measure changes in depressive symptoms in children ages 6 to 12, but its validity and reliability have also been demonstrated in the adolescent population (up to 18 years old). Covering 17 symptom areas, the scale was adapted from the Hamilton Depression Rating Scale and is set up as a semi-structured interview with the child/adolescent. It takes 10 to 15 minutes to administer and score.
Poznanski, E.O., Cook, S.C., & Carroll, B.J. (1979). A depression rating scale for children. Pediatrics, 64(4), 442-450.
Poznanski, E.O., & Mokros, H.B. (1996). Children's depression rating scale, revised (CDRS-R). Los Angeles: Western Psychological Services.

Mayes, T.L., Bernstein, I.H., Haley, C.L., Kennard, B.D., & Emslie, G.J. (2010). Psychometric properties of the children's depression rating scale–revised in adolescents. Journal of Child and Adolescent Psychopharmacology, 20(6), 513-516. https://doi.org/ 10.1089/cap.2010.0063
More Information
How to Access
- Pricing varies and can be purchased through Western Psychological Services Publishing.
General Adult Population
The Beck Hopelessness Scale is a self-report measure for adults age 17 to 80. It assesses an individual’s negative expectations about the future. The measure includes 20 items to which participants respond with “true” or “false.” It takes five to 10 minutes to complete.
Beck, A.T., Weissman, A., Lester, D., & Trexler, L. (1974). The measurement of pessimism: The Hopelessness Scale. Journal of Consulting and Clinical Psychology, 42(6), 861-865. http://dx.doi.org/10.1037/h0037562
Beck, A.T., & Steer, R.A. (1988). Manual for the Beck Hopelessness Scale. San Antonio: Psychological Corp.
Neufeld, E., O'Rourke, N., & Donnelly, M. (2010). Enhanced measurement sensitivity of hopeless ideation among older adults at risk of self-harm: Reliability and validity of likert-type responses to the Beck Hopelessness Scale. Aging & Mental Health, 14(6), 752-756. http://dx.doi.org/10.1080/13607860903421052
More Information
How to Access
- Pricing varies and can be purchased through Pearson Assessments.
Quick Inventory of Depressive Symptomatology-Self-Report (QIDS-SR)
The QIDS-SR measures the severity of depressive symptoms in adults 18 and older. There are 16 measures, selected from the Inventory of Depressive Symptomology (IDS, 2000). These symptoms correspond to the diagnostic criteria from the DSM-IV. Respondents use a 4-point Likert-type scale to assess their behaviors and mood over the course of the past week. It takes five to seven minutes to complete the report.
Rush, A.J., Trivedi, M.H., Ibrahim, H.M., Carmody, T.J., Arnow, B., Klein, D.N., . . . Keller, M.B. (2003). The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573-583. http://dx.doi.org/10.1016/S0006-3223(02)01866-8

More Information
How to Access
- Pricing varies and can be purchased through ePROVIDE Mapi Research TrustTM.
- An electronic version is also available through MD+CALC.
The Patient Health Questionnaire (PHQ) is a self-report measure designed to screen depressive symptoms. It takes one to five minutes to complete and roughly the same amount of time for a clinician to review the responses. The PHQ-9 is available in multiple languages.
Spitzer, R.L., Kroenke, K., Williams, J.B.W., & Patient Health Questionnaire Primary Care Study Group. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA: Journal of the American Medical Association, 282(18), 1737-1744. http://dx.doi.org/10.1001/jama.282.18.1737
Kroenke, K., Spitzer, R.L., & Williams, J.B.W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606-613. http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x
Martin, A., Rief, W., Klaiberg, A., & Braehler, E. (2006). Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. General Hospital Psychiatry, 28(1), 71-77. https://doi.org/10.1016/j.genhosppsych.2005.07.003
More Information
How to Access
- The PHQ-9 (PDF, 41KB) is in the public domain and no permission is required for use.
The Reminiscence Functions Scale (RFS) is a 43-item questionnaire that takes 15 to 25 minutes to complete. The RFS assesses the frequency with which adults, 18 years and older, engage in the act of recollecting past experiences or events. Respondents answer questions on a 6-point Likert-type scale, and responses are scored in eight different categories.
Webster, J.D. (1993). Construction and validation of the Reminiscence Functions Scale. Journal of Gerontology, 48(5), P256-P262. http://dx.doi.org/10.1093/geronj/48.5.P256
Robitaille, A., Cappeliez, P., Coulombe, D., & Webster, J.D. (2010). Factorial structure and psychometric properties of the reminiscence functions scale. Aging & Mental Health, 14(2), 184-192. https://doi.org/10.1080/13607860903167820
More Information
How to Access
Used by permission from Dr. Jeffrey Webster.
As part of the Medical Outcomes Study (MOS), a multi-year, multi-site study that investigated variations in patient outcomes, the RAND Corporation developed the 36-item Short Form Health Survey (SF-36) as a set of easily administered quality-of-life measures. These measures rely on patient self-reports and are widely used for routine monitoring and assessment of care outcomes in the adult population. The survey can be completed in 10 minutes or less.
Ware, J.E., & Sherbourne, C.D. (1992). The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care, 30(6), 473-483. http://dx.doi.org/10.1097/00005650-199206000-00002
McHorney, C.A., Ware Jr, J.E., Lu, J.R., & Sherbourne, C.D. (1994). The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32(1), 40-66. Retrieved from http://www.jstor.org/stable/3766189
More Information
How to Access
The Social Adjustment Scale (SAS-SR) is a self-report measure of social functioning. It contains 54 items rated on a 5-point scale. It takes about 20 minutes to complete and is intended for individuals 17 years and older. There are also Short and Screener versions available, which take five to 10 minutes to complete.
Weissman, M.M., & Bothwell, S. (1976). Assessment of social adjustment by patient self-report. Archives of General Psychiatry, 33(9), 1111-1115. https://doi.org/10.1001/archpsyc.1976.01770090101010
Gameroff, M.J., Wickramaratne, P., & Weissman, M.M. (2012). Testing the Short and Screener versions of the Social Adjustment Scale–Self‐report (SAS‐SR). International Journal of Methods in Psychiatric Research, 21(1), 52-65. https://doi.org/10.1002/mpr.358
More Information
How to Access
- Pricing varies and can be purchased through MHS Assessments.
The Social Functioning Questionnaire (SFQ) is a self-report tool that measures social functioning in adults over the last two weeks. The questionnaire contains eight questions which are rated on a 4-point scale. It takes less than four minutes to complete.
Tyrer, P., Nur, U., Crawford, M., Karlsen, S., McLean, C., Rao, B., & Johnson, T. (2005). The social functioning questionnaire: A rapid and robust measure of perceived functioning. International Journal of Social Psychiatry, 51(3), 265-275. http://dx.doi.org/10.1177/0020764005057391
More Information
How to Access
© 2005 by SAGE Publications. Reproduced by Permission of SAGE Publications.
Older Adults
Geriatric Depression Scale (GDS)
The Geriatric Depression Scale (GDS) is specifically designed to screen and measure depression in older adults. It contains 30 forced-choice “yes” or “no” questions, a format that is helpful for individuals with cognitive dysfunction. Questions relate to how an individual has felt in a specified time frame. It takes five to seven minutes to complete the questionnaire.
Yesavage, J.A., Brink, T.L., Rose, T.L., Lum, O., Huang, V., Adey, M., & Leirer, V.O. (1982-1983). Development and validation of a Geriatric Depression Screening Scale: A preliminary report. Journal of Psychiatric Research, 17(1), 37-49. http://dx.doi.org/10.1016/0022-3956(82)90033-4
Lopez, M.N., Quan, N.M., & Carvajal, P.M. (2010). A psychometric study of the Geriatric Depression Scale. European Journal of Psychological Assessment, 26(1), 55-60. http://dx.doi.org/10.1027/1015-5759/a000008
More Information
How to Access
- The GDS is in the public domain and no permission is required for use. A copy of the instrument is available either electronically or as plain text through Stanford University.
Also called the Life Satisfaction Ratings (LSR), the Life Satisfaction Index is designed to measure well-being and successful aging among adults over the age of 50. It is administered by a health care professional. There are five categories that are rated on a 5-point scale. The estimated time for completing the questionnaire is 10 minutes.
Neugarten, B.J., Havighurst, R.J., & Tobin, S.S. (1961). The measurement of life satisfaction. Journal of Gerontology, 16, 134-143. http://dx.doi.org/10.1093/geronj/16.2.134
Adams, D.L. (1969). Analysis of a life satisfaction index. Journal of Gerontology, 24(4), 470-474. https://doi.org/10.1093/geronj/24.4.470
Barrett, A.J., & Murk, P.J. (2006). Life satisfaction index for the third age (LSITA): A measurement of successful aging. In E. P. Isaac (Ed.), Proceedings of the 2006 Midwest research-to-practice conference in adult, continuing, and community education (pp. 7-12). St. Louis: University of Missouri-St. Louis.
More Information
Used by permission. Published by Oxford University Press on behalf of The Gerontological Society of America.
How to Access
Other investigators may use the scales and indexes reproduced in this report without permission from either the present investigators or the Journal of Gerontology.
| Beck Depression Inventory | |
|---|---|
| Purpose | measure severity of depression |
The Beck Depression Inventory (BDI, BDI-1A, BDI-II), created by Aaron T. Beck, is a 21-question multiple-choiceself-report inventory, one of the most widely used psychometric tests for measuring the severity of depression. Its development marked a shift among mental health professionals, who had until then, viewed depression from a psychodynamic perspective, instead of it being rooted in the patient's own thoughts.
In its current version, the BDI-II is designed for individuals aged 13 and over, and is composed of items relating to symptoms of depression such as hopelessness and irritability, cognitions such as guilt or feelings of being punished, as well as physical symptoms such as fatigue, weight loss, and lack of interest in sex.[1]
There are three versions of the BDI—the original BDI, first published in 1961 and later revised in 1978 as the BDI-1A, and the BDI-II, published in 1996. The BDI is widely used as an assessment tool by health care professionals and researchers in a variety of settings.
The BDI was used as a model for the development of the Children's Depression Inventory (CDI), first published in 1979 by clinical psychologist Maria Kovacs.[2]
Development and history[edit]
According to Beck's publisher, 'When Beck began studying depression in the 1950s, the prevailing psychoanalytic theory attributed the syndrome to inverted hostility against the self.'[3] By contrast, the BDI was developed in a novel way for its time; by collating patients' verbatim descriptions of their symptoms and then using these to structure a scale which could reflect the intensity or severity of a given symptom.[1]
Beck drew attention to the importance of 'negative cognitions' described as sustained, inaccurate, and often intrusive negative thoughts about the self.[4] In his view, it was the case that these cognitions caused depression, rather than being generated by depression.
Beck developed a triad of negative cognitions about the world, the future, and the self, which play a major role in depression.An example of the triad in action taken from Brown (1995) is the case of a student obtaining poor exam results:
- The student has negative thoughts about the world, so he may come to believe he does not enjoy the class.
- The student has negative thoughts about his future because he thinks he may not pass the class.
- The student has negative thoughts about his self, as he may feel he does not deserve to be in college.[5]
The development of the BDI reflects that in its structure, with items such as 'I have lost all of my interest in other people' to reflect the world, 'I feel discouraged about the future' to reflect the future, and 'I blame myself for everything bad that happens' to reflect the self. The view of depression as sustained by intrusive negative cognitions has had particular application in cognitive behavioral therapy (CBT), which aims to challenge and neutralize them through techniques such as cognitive restructuring.
BDI[edit]
The original BDI, first published in 1961,[6] consisted of twenty-one questions about how the subject has been feeling in the last week. Each question had a set of at least four possible responses, ranging in intensity. For example:
- (0) I do not feel sad.
- (1) I feel sad.
- (2) I am sad all the time and I can't snap out of it.
- (3) I am so sad or unhappy that I can't stand it.
Beck Hopelessness Scale Questionnaire Online
When the test is scored, a value of 0 to 3 is assigned for each answer and then the total score is compared to a key to determine the depression's severity. The standard cut-off scores were as follows:[7]
- 0–9: indicates minimal depression
- 10–18: indicates mild depression
- 19–29: indicates moderate depression
- 30–63: indicates severe depression.
Higher total scores indicate more severe depressive symptoms.
Some items on the original BDI had more than one statement marked with the same score. For instance, there are two responses under the Mood heading that score a 2: (2a) 'I am blue or sad all the time and I can't snap out of it' and (2b) 'I am so sad or unhappy that it is very painful'.[1]
BDI-IA[edit]
The BDI-IA was a revision of the original instrument developed by Beck during the 1970s, and copyrighted in 1978. To improve ease of use, the 'a and b statements' described above were removed, and respondents were instructed to endorse how they had been feeling during the preceding two weeks.[8][9] The internal consistency for the BDI-IA was good, with a Cronbach's alpha coefficient of around 0.85, meaning that the items on the inventory are highly correlated with each other.[10]
However, this version retained some flaws; the BDI-IA only addressed six out of the nine DSM-III criteria for depression. This and other criticisms were addressed in the BDI-II.
BDI-II[edit]
The BDI-II was a 1996 revision of the BDI,[9] developed in response to the American Psychiatric Association's publication of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, which changed many of the diagnostic criteria for Major Depressive Disorder.
Items involving changes in body image, hypochondriasis, and difficulty working were replaced. Also, sleep loss and appetite loss items were revised to assess both increases and decreases in sleep and appetite. All but three of the items were reworded; only the items dealing with feelings of being punished, thoughts about suicide, and interest in sex remained the same. Finally, participants were asked to rate how they have been feeling for the past two weeks, as opposed to the past week as in the original BDI.
Beck Hopelessness Scale Questionnaire Online
Like the BDI, the BDI-II also contains 21 questions, each answer being scored on a scale value of 0 to 3. Higher total scores indicate more severe depressive symptoms. The standardized cutoffs used differ from the original:
- 0–13: minimal depression
- 14–19: mild depression
- 20–28: moderate depression
- 29–63: severe depression.[11]
One measure of an instrument's usefulness is to see how closely it agrees with another similar instrument that has been validated against information from a clinical interview by a trained clinician. In this respect, the BDI-II is positively correlated with the Hamilton Depression Rating Scale with a Pearson r of 0.71, showing good agreement. The test was also shown to have a high one-week test–retest reliability (Pearson r =0.93), suggesting that it was not overly sensitive to daily variations in mood.[12] The test also has high internal consistency (α=.91).[9]
Impact[edit]
The development of the BDI was an important event in psychiatry and psychology; it represented a shift in health care professionals' view of depression from a Freudian, psychodynamic perspective, to one guided by the patient's own thoughts or 'cognitions'.[3] It also established the principle that instead of attempting to develop a psychometric tool based on a possibly invalid theory, self-report questionnaires when analysed using techniques such as factor analysis can suggest theoretical constructs.
The BDI was originally developed to provide a quantitative assessment of the intensity of depression. Because it is designed to reflect the depth of depression, it can monitor changes over time and provide an objective measure for judging improvement and the effectiveness or otherwise of treatment methods.[13] The instrument remains widely used in research; in 1998, it had been used in over 2000 empirical studies.[14] It has been translated into multiple European languages as well as Arabic, Chinese, Japanese, Persian,[15] and Xhosa.[16]
Limitations[edit]
The BDI suffers from the same problems as other self-report inventories, in that scores can be easily exaggerated or minimized by the person completing them. Like all questionnaires, the way the instrument is administered can have an effect on the final score. If a patient is asked to fill out the form in front of other people in a clinical environment, for instance, social expectations have been shown to elicit a different response compared to administration via a postal survey.[17]
In participants with concomitant physical illness the BDI's reliance on physical symptoms such as fatigue may artificially inflate scores due to symptoms of the illness, rather than of depression.[18] In an effort to deal with this concern Beck and his colleagues developed the 'Beck Depression Inventory for Primary Care' (BDI-PC), a short screening scale consisting of seven items from the BDI-II considered to be independent of physical function. Unlike the standard BDI, the BDI-PC produces only a binary outcome of 'not depressed' or 'depressed' for patients above a cutoff score of 4.[19]
Although designed as a screening device rather than a diagnostic tool, the BDI is sometimes used by health care providers to reach a quick diagnosis.[20]
The BDI is copyrighted; a fee must be paid for each copy used. There is no evidence that the BDI-II is more valid or reliable than other depression scales,[21] and public domain scales such as the Patient Health Questionnaire – Nine Item (PHQ-9) have been studied as a useful tool.[22]
See also[edit]
Notes[edit]
- ^ abcBeck AT (1972). Depression: Causes and Treatment. Philadelphia: University of Pennsylvania Press. ISBN0-8122-1032-8.
- ^Kovacs, M. (1992). Children's Depression Inventory. North Tonawanda, NY: Multi-Health Systems, Inc.
- ^ abMcGraw Hill Publishing Company 'Test developer profile: Aaron T. Beck'.Retrieved on 2009-02-24Aaron T. Beck, M.D. at the Wayback Machine (archived 17 March 2009)
- ^Allen JP (2003). 'An Overview of Beck's Cognitive Theory of Depression in Contemporary Literature'. Retrieved 2004-02-24.
- ^Brown GP, Hammen CL, Craske MG, Wickens TD (August 1995). 'Dimensions of dysfunctional attitudes as vulnerabilities to depressive symptoms'. Journal of Abnormal Psychology. 104 (3): 431–5. doi:10.1037/0021-843X.104.3.431. PMID7673566. Retrieved 2008-10-30.
- ^Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (June 1961). 'An inventory for measuring depression'. Arch. Gen. Psychiatry. 4 (6): 561–71. doi:10.1001/archpsyc.1961.01710120031004. PMID13688369.
- ^Beck AT, Steer RA, Garbin MG J (1988). 'Psychometric properties of the Beck Depression Inventory Twenty-five years of evaluation'. Clin. Psychol. Rev. 8: 77–100. doi:10.1016/0272-7358(88)90050-5.
- ^Moran PW, Lambert MJ (1983). 'A review of current assessment tools for monitoring changes in depression'. In Lambert MS, Christensen ER, DeJulio S (eds.). The Assessment of Psychotherapy Outcomes. New York: Wiley.
- ^ abcBeck AT, Steer RA, Ball R, Ranieri W (December 1996). 'Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients'. Journal of Personality Assessment. 67 (3): 588–97. doi:10.1207/s15327752jpa6703_13. PMID8991972. Retrieved 2008-10-30.
- ^Ambrosini PJ, Metz C, Bianchi MD, Rabinovich H, Undie A (January 1991). 'Concurrent validity and psychometric properties of the Beck Depression Inventory in outpatient adolescents'. Journal of the American Academy of Child and Adolescent Psychiatry. 30 (1): 51–7. doi:10.1097/00004583-199101000-00008. PMID2005064. Retrieved 2008-10-30.
- ^https://www.psychcongress.com/saundras-corner/scales-screenersdepression/beck-depression-inventory-ii-bdi-ii
- ^Beck AT, Steer RA and Brown GK (1996) 'Manual for the Beck Depression Inventory-II'. San Antonio, TX: Psychological Corporation
- ^Beck AT, Ward C, Mendelson M (1961). 'Beck Depression Inventory (BDI)'. Arch Gen Psychiatry. 4 (6): 561–571. doi:10.1001/archpsyc.1961.01710120031004. PMID13688369.
- ^Richter, P; J Werner; A Heerlein; A Kraus; H Sauer (1998). 'On the validity of the Beck Depression Inventory. A review'. Psychopathology. 31 (3): 160–8. doi:10.1159/000066239. ISSN0254-4962. PMID9636945.
- ^'Literature available on Psychiatric Assessment Instruments translated in non-English languages: TBDI Section'. Victorian Transcultural Psychiatry Unit. December 2005. Archived from the original on July 19, 2008. Retrieved 2009-02-24.
- ^Steele GI (October 2006). 'The development and validation of the Xhosa translations of the Beck Depression Inventory, the Beck Anxiety Inventory, and the Beck Hopelessness Scale'. biblioteca universia. Archived from the original on 2011-07-25. Retrieved 2009-02-24.
- ^Bowling A (September 2005). 'Mode of questionnaire administration can have serious effects on data quality'. Journal of Public Health. 27 (3): 281–91. doi:10.1093/pubmed/fdi031. PMID15870099.
- ^Moore MJ, Moore PB, Shaw PJ (October 1998). 'Mood disturbances in motor neurone disease'. Journal of the Neurological Sciences. 160 Suppl 1: S53–6. doi:10.1016/S0022-510X(98)00203-2. PMID9851650.
- ^Steer RA, Cavalieri TA, Leonard DM, Beck AT (1999). 'Use of the Beck Depression Inventory for Primary Care to screen for major depression disorders'. General Hospital Psychiatry. 21 (2): 106–11. doi:10.1016/S0163-8343(98)00070-X. PMID10228890.
- ^Hersen M, Turner SM, Beidel DC (2007). Adult Psychopathology and Diagnosis (5th ed.). John Wiley & Sons. pp. 301–302. ISBN978-0-471-74584-6.
- ^ZimmermanM. Using scales to monitor symptoms and treatment of depression (measurement based care). In UpToDate, Rose, BD (Ed), UpToDate, Waltham, MA, 2011.
- ^Kroenke K, Spitzer RL, Williams JB (September 2001). 'The PHQ-9: Validity of a Brief Depression Severity Measure'. J Gen Intern Med. 16 (9): 606–13. doi:10.1046/j.1525-1497.2001.016009606.x. PMC1495268. PMID11556941.
Further reading[edit]
- Beck A.T. (1988). 'Beck Hopelessness Scale.' The Psychological Corporation.
- Craven J, Rodin G, Littlefield C (1988). 'The Beck Depression Inventory as a screening device for major depression in renal dialysis patients'. Int J Psychiatry Med. 18 (4): 365–374. doi:10.2190/M1TX-V1EJ-E43L-RKLF. PMID3235282.